Deep vein thrombosis (DVT) is a serious medical condition that affects the veins deep within your body, often in the legs. The condition occurs when a blood clot forms in a deep vein, which can disrupt blood flow and cause severe complications, such as a pulmonary embolism (PE), when the clot breaks loose and travels to the lungs. Recognizing deep vein thrombosis symptoms early is key to preventing such life-threatening events.
In this article, we will explore the various deep vein thrombosis symptoms, risk factors, causes, and the importance of seeking timely medical intervention. By understanding the signs, you can protect yourself and your loved ones from the potentially dangerous consequences of DVT.
What is Deep Vein Thrombosis?
Deep vein thrombosis (DVT) occurs when a blood clot forms in one of the deep veins, typically in the lower leg, thigh, or pelvis. These clots can block the normal flow of blood and lead to swelling, pain, and sometimes severe complications. While DVT itself may not always present noticeable symptoms, the formation of the clot can result in several key signs that should not be ignored.
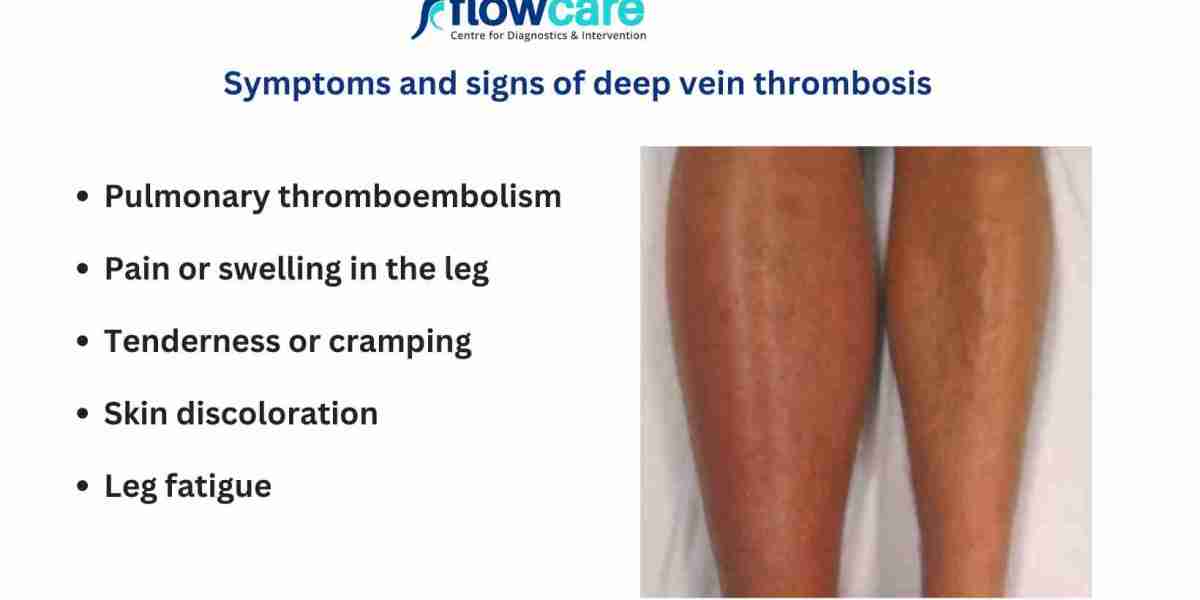
Common Symptoms of Deep Vein Thrombosis
Recognizing deep vein thrombosis symptoms early can help reduce the risk of severe complications. Common symptoms include:
1. Swelling in One Leg
Swelling, especially in one leg, is one of the most common symptoms of DVT. The affected leg may feel heavy, tight, or appear visibly enlarged due to the clot blocking blood flow. This swelling might not go away with elevation or compression.
2. Pain or Tenderness
Pain or tenderness in the affected area, particularly in the calf or thigh, is another hallmark of DVT. The pain can range from mild to severe and is usually worsened when standing or walking. In some cases, the pain may feel like cramping or soreness.
3. Warmth and Redness
When a clot forms in the vein, the area around it can become warm to the touch. Additionally, the skin over the clot may become red or discolored. This occurs due to inflammation and the restriction of blood flow to the affected area.
4. Swollen Veins
In some cases, the veins near the skin surface may become more visible and engorged. These veins appear swollen or distorted due to the buildup of blood behind the clot.
5. Leg Pain When Standing or Walking
If you notice a sharp or aching pain in the affected leg, particularly when standing or walking, this may indicate the presence of DVT. The discomfort often worsens when the leg is in a stationary position for extended periods.
6. Skin Discoloration
The skin around the clot may take on a bluish or reddish hue, reflecting changes in blood flow and oxygenation due to the clot. This discoloration can be an important indicator of the condition.
Risk Factors for Developing DVT
Several factors can increase your risk of developing deep vein thrombosis, including:
- Prolonged immobility: Being sedentary for long periods, such as during long flights or bed rest after surgery, increases the likelihood of clot formation.
- Age: People over 60 are at a higher risk of developing DVT.
- Obesity: Excess weight puts additional pressure on your veins, making it more difficult for blood to flow properly.
- Pregnancy: Pregnancy increases the pressure on veins in the pelvic area, contributing to the risk of DVT.
- Smoking: Smoking can damage blood vessels and increase the likelihood of clot formation.
- Previous DVT: If you have had a DVT episode in the past, your risk of developing another clot increases.
- Certain medical conditions: Conditions like heart disease, cancer, or autoimmune disorders can elevate the risk of DVT.
How is Deep Vein Thrombosis Diagnosed?
If you experience deep vein thrombosis symptoms, it’s important to consult a healthcare provider as soon as possible. The diagnosis of DVT often involves several steps:
- Physical Exam: The doctor will assess the affected area for signs of swelling, tenderness, or redness.
- Ultrasound: An ultrasound is the most common test used to diagnose DVT. It uses sound waves to create an image of the clot and helps to confirm its presence.
- Blood Tests: A blood test, known as a D-dimer test, can help indicate whether a clot is present. Elevated levels of D-dimer suggest the possibility of a clot, but further tests are needed for confirmation.
- Venography: In rare cases, a venogram may be performed, which involves injecting a contrast dye into the veins to reveal the clot on an X-ray.
Complications of Deep Vein Thrombosis
If left untreated, DVT can lead to serious complications:
1. Pulmonary Embolism (PE)
A pulmonary embolism occurs when a blood clot breaks free from its original location and travels to the lungs, blocking a pulmonary artery. This can be life-threatening, causing difficulty breathing, chest pain, or even sudden death.
2. Post-Thrombotic Syndrome
Some people who have had DVT develop post-thrombotic syndrome, a condition that causes chronic pain, swelling, and heaviness in the affected limb. It may occur months or even years after the clot forms and can significantly affect your quality of life.
3. Chronic Venous Insufficiency
DVT can cause damage to the veins, leading to chronic venous insufficiency. This condition impairs the ability of the veins to return blood to the heart, leading to swelling, pain, and skin changes in the affected area.
Treatment for Deep Vein Thrombosis
The treatment for DVT aims to prevent the clot from growing, prevent it from breaking loose, and reduce the risk of complications. Common treatment options include:
1. Blood Thinners
Blood thinners (anticoagulants) are the primary treatment for DVT. These medications help prevent further clotting and reduce the risk of the clot traveling to other parts of the body.
2. Compression Stockings
Compression stockings help reduce swelling and prevent blood from pooling in the veins. They provide gentle pressure to promote better circulation in the affected leg.
3. Thrombectomy
In some cases, when the clot is large or causing significant symptoms, a thrombectomy (clot removal) may be performed. This procedure is often done in emergency situations.
4. Inferior Vena Cava (IVC) Filter
In people who cannot take blood thinners, a filter may be placed in the inferior vena cava (a large vein in the abdomen) to catch any clots that break free and prevent them from reaching the lungs.
Prevention of Deep Vein Thrombosis
Prevention is key when it comes to DVT. Here are some tips to reduce your risk:
- Stay active: Regular physical activity, such as walking or swimming, helps improve circulation.
- Take breaks: If you’re sitting for extended periods (e.g., during long flights), take breaks to stand up and stretch your legs.
- Wear compression stockings: These can help prevent blood from pooling in your legs, particularly during long periods of immobility.
- Maintain a healthy weight: Reducing your weight lowers the pressure on your veins and reduces your risk.
- Stay hydrated: Dehydration can increase the risk of clot formation, so drinking enough water is important.
Conclusion
Recognizing deep vein thrombosis symptoms early is crucial in preventing the potentially severe complications that can arise from the condition. If you notice any signs of DVT, such as swelling, pain, or redness in one leg, it’s important to seek medical attention right away. By understanding the symptoms and taking steps to manage risk factors, you can help reduce your chances of developing DVT and protect your health.